
Breaking News
 Why Dual Engine Failure Changes Everything -- Louisville Crash Update
Why Dual Engine Failure Changes Everything -- Louisville Crash Update
 Transforming Storage Shelf / Workbench - Small Space Organization
Transforming Storage Shelf / Workbench - Small Space Organization
 Our 3-Step Strategy for a Stress-Free Pantry
Our 3-Step Strategy for a Stress-Free Pantry
 BEHIND THE DEEP STATE | The War on Farms
BEHIND THE DEEP STATE | The War on Farms
Top Tech News
 HUGE 32kWh LiFePO4 DIY Battery w/ 628Ah Cells! 90 Minute Build
HUGE 32kWh LiFePO4 DIY Battery w/ 628Ah Cells! 90 Minute Build
 What Has Bitcoin Become 17 Years After Satoshi Nakamoto Published The Whitepaper?
What Has Bitcoin Become 17 Years After Satoshi Nakamoto Published The Whitepaper?
 Japan just injected artificial blood into a human. No blood type needed. No refrigeration.
Japan just injected artificial blood into a human. No blood type needed. No refrigeration.
 The 6 Best LLM Tools To Run Models Locally
The 6 Best LLM Tools To Run Models Locally
 Testing My First Sodium-Ion Solar Battery
Testing My First Sodium-Ion Solar Battery
 A man once paralyzed from the waist down now stands on his own, not with machines or wires,...
A man once paralyzed from the waist down now stands on his own, not with machines or wires,...
 Review: Thumb-sized thermal camera turns your phone into a smart tool
Review: Thumb-sized thermal camera turns your phone into a smart tool
 Army To Bring Nuclear Microreactors To Its Bases By 2028
Army To Bring Nuclear Microreactors To Its Bases By 2028
 Nissan Says It's On Track For Solid-State Batteries That Double EV Range By 2028
Nissan Says It's On Track For Solid-State Batteries That Double EV Range By 2028
Hormonal Contraception Linked to Increased Breast Cancer Risk in BRCA1 Carriers
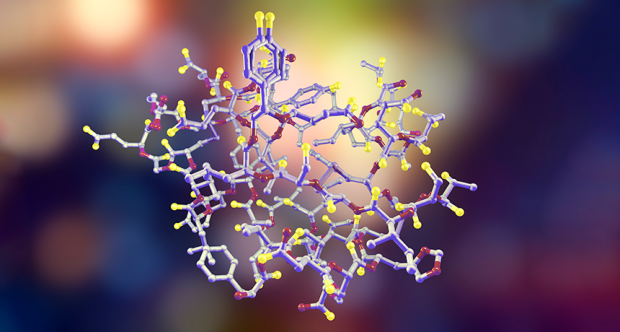
Carriers of the BRCA1 cancer gene had a significantly increased risk of breast cancer if they used hormonal contraception (HC), pooled cohort data showed.
Breast cancer risk increased by 29% in BRCA1 carriers who reported any use of HC during at least one 12-month continuous period. The risk also increased with duration of HC use, but separate analyses showed no increased risk associated with current use within the past year, 1-5 years in the past, 6-10 years before, or more than 10 years.
The analysis showed no evidence of increased breast cancer risk for BRCA2 carriers who used HC, reported Kelly-Anne Phillips, MD, MBBS, of Peter MacCallum Cancer Center in Melbourne, Australia, and co-authors in the Journal of Clinical Oncologyopens in a new tab or window.
"When counseling women, absolute risks are more useful than relative risks," the authors noted in their discussion of the findings. "These absolute risks will be different for different women, so incorporating our findings into risk prediction models such as CanRiskopens in a new tab or window would assist in providing personalized estimates."
"Decisions about use of HC in women at increased risk for BC [breast cancer] due to BRCA1 mutations need to carefully weigh the absolute risks and benefits," they added. "While shorter-term use may result in only small increases, prolonged cumulative use may result in larger increases in absolute BC risk that may not be acceptable to some women."
An individualized approach to patient counseling about breast cancer risk in BRCA1 carriers is advisable, agreed Yara Abdou, MD, of the University of North Carolina and Lineberger Comprehensive Cancer Center in Chapel Hill.
"These results suggest that for BRCA1 mutation carriers, HC use should be approached with caution, particularly for prolonged durations," Abdou told MedPage Today via email. "Clinicians should engage in detailed risk-benefit discussions with BRCA1 carriers considering HC use, emphasizing the potential increased risk of breast cancer."
"For BRCA2 carriers, the lack of a significant association suggests a lower risk; however, the relatively small number of breast cancer cases in this group warrants cautious interpretation."
The observational design of the study limits the ability to establish a causal relationship between HC use and breast cancer in BRCA1 carriers, Abdou noted. Additionally, the median follow-up of 5.9 years for BRCA1 carriers and 5.6 years for BRCA2 carriers might not be long enough to capture the long-term effects of HC use on breast cancer risk.

 Carbon based computers that run on iron
Carbon based computers that run on iron

