
Breaking News
 BANK OF AMERICA SURRENDERS: BofA Just Issued a $309 Silver Alert (Physical Premiums Exploding)
BANK OF AMERICA SURRENDERS: BofA Just Issued a $309 Silver Alert (Physical Premiums Exploding)
 Steve Witkoff says they are close to finishing "a prosperity agreement" for Ukraine,...
Steve Witkoff says they are close to finishing "a prosperity agreement" for Ukraine,...
 NOW - Starmer says a declaration of intent has been signed...
NOW - Starmer says a declaration of intent has been signed...
 Remarks at the New Jersey Bankers Association, Jersey City, New Jersey
Remarks at the New Jersey Bankers Association, Jersey City, New Jersey
Top Tech News
 The First Production All-Solid-State Battery Is Here, And It Promises 5-Minute Charging
The First Production All-Solid-State Battery Is Here, And It Promises 5-Minute Charging
 See inside the tech-topia cities billionaires are betting big on developing...
See inside the tech-topia cities billionaires are betting big on developing...
 Storage doesn't get much cheaper than this
Storage doesn't get much cheaper than this
 Laser weapons go mobile on US Army small vehicles
Laser weapons go mobile on US Army small vehicles
 EngineAI T800: Born to Disrupt! #EngineAI #robotics #newtechnology #newproduct
EngineAI T800: Born to Disrupt! #EngineAI #robotics #newtechnology #newproduct
 This Silicon Anode Breakthrough Could Mark A Turning Point For EV Batteries [Update]
This Silicon Anode Breakthrough Could Mark A Turning Point For EV Batteries [Update]
 Travel gadget promises to dry and iron your clothes – totally hands-free
Travel gadget promises to dry and iron your clothes – totally hands-free
 Perfect Aircrete, Kitchen Ingredients.
Perfect Aircrete, Kitchen Ingredients.
 Futuristic pixel-raising display lets you feel what's onscreen
Futuristic pixel-raising display lets you feel what's onscreen
 Cutting-Edge Facility Generates Pure Water and Hydrogen Fuel from Seawater for Mere Pennies
Cutting-Edge Facility Generates Pure Water and Hydrogen Fuel from Seawater for Mere Pennies
MIT's "living drug factories" produce insulin from inside the body
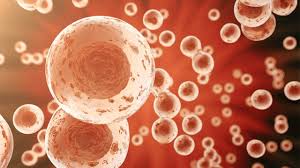
For the last couple of decades, a relatively small amount of diabetics have benefited from what's known as pancreatic islet cell transplantation. These are the cells that produce insulin in a functional pancreas and by implanting them into sufferers of diabetes, they can take on their traditional role and negate the need for regular insulin injections.
The reason this form of therapy isn't used more widely is that the great majority of recipients experience complications, as their immune system mistakes the transplanted cells for dangerous invaders and goes on the attack. Drugs that suppress this immune response are one solution, but they invite their own risks such as vulnerability to infection or more serious side effects.
So getting pancreatic islet cells to survive transplantation and function as normal is seen as a key objective by researchers in the field. Converting the patient's own liver cells into islet cells, wrapping them in seaweed-based capsules and organizing them into clusters are just a few of the ways the process may be improved, and now scientists at MIT have come up with another.
The technology involves encapsulating the cells in a protective shell made from a silicon-based elastomer, combined with a porous membrane. These pores are large enough that nutrients, oxygen and insulin can move freely through the membrane, but small enough to keep out immune cells that seek to attack the cell.



