
Breaking News
 Trump and Netanyahu Meet Again
Trump and Netanyahu Meet Again
 Doug Casey's Top Prediction for 2026… What It Means for You and Your Money
Doug Casey's Top Prediction for 2026… What It Means for You and Your Money
 If Independent Agencies Are Unconstitutional, so Is the Fed
If Independent Agencies Are Unconstitutional, so Is the Fed
 Quantum walkie-talkie: China tests world's first GPS-free radio for border zones
Quantum walkie-talkie: China tests world's first GPS-free radio for border zones
Top Tech News
 EngineAI T800: Born to Disrupt! #EngineAI #robotics #newtechnology #newproduct
EngineAI T800: Born to Disrupt! #EngineAI #robotics #newtechnology #newproduct
 This Silicon Anode Breakthrough Could Mark A Turning Point For EV Batteries [Update]
This Silicon Anode Breakthrough Could Mark A Turning Point For EV Batteries [Update]
 Travel gadget promises to dry and iron your clothes – totally hands-free
Travel gadget promises to dry and iron your clothes – totally hands-free
 Perfect Aircrete, Kitchen Ingredients.
Perfect Aircrete, Kitchen Ingredients.
 Futuristic pixel-raising display lets you feel what's onscreen
Futuristic pixel-raising display lets you feel what's onscreen
 Cutting-Edge Facility Generates Pure Water and Hydrogen Fuel from Seawater for Mere Pennies
Cutting-Edge Facility Generates Pure Water and Hydrogen Fuel from Seawater for Mere Pennies
 This tiny dev board is packed with features for ambitious makers
This tiny dev board is packed with features for ambitious makers
 Scientists Discover Gel to Regrow Tooth Enamel
Scientists Discover Gel to Regrow Tooth Enamel
 Vitamin C and Dandelion Root Killing Cancer Cells -- as Former CDC Director Calls for COVID-19...
Vitamin C and Dandelion Root Killing Cancer Cells -- as Former CDC Director Calls for COVID-19...
 Galactic Brain: US firm plans space-based data centers, power grid to challenge China
Galactic Brain: US firm plans space-based data centers, power grid to challenge China
Giving T cells extra batteries supercharges them against cancer
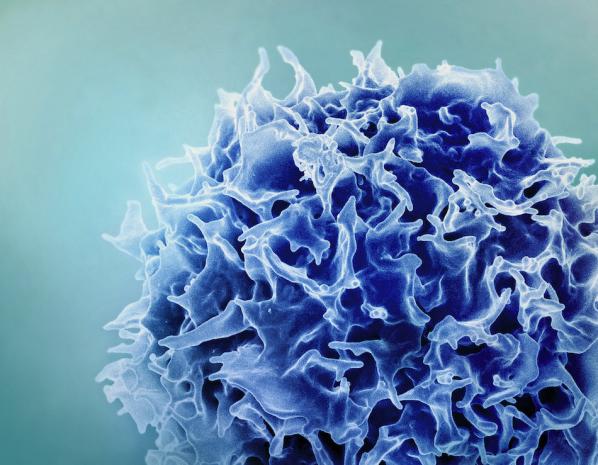
In a fair fight, the immune system would wipe out cancer every time – but this crafty disease doesn't play fair. Along with its many tricks to avoid detection, tumors build microenvironments around themselves that are toxic to immune cells, draining them of energy. Sustained immune responses against a pathogen like cancer can lead to T cell exhaustion.
Finding ways to supercharge the immune system to continue the fight is the main goal of immunotherapy. Now, a team from Brigham and Women's Hospital has demonstrated a new way to refresh T cells, by essentially replacing their batteries.
Mitochondria are organelles that produce chemical energy for cells, but during T cell exhaustion these little batteries can be lost or damaged. Previous studies have shown that cancer cells can use nanotubes like "tiny tentacles" to slurp up mitochondria from immune cells. For the new study, the researchers found that they could use the same mechanism to do the opposite – donate new mitochondria to T cells, from bone marrow stromal cells (BMSCs).
The team cultured BMSCs and T cells together, and after 48 hours found that up to a quarter of the T cells had gained extra mitochondria. The researchers dubbed these juiced up immune cells Mito+.
In tests in mice, Mito+ cells were found to more easily penetrate tumors and launch a more robust attack on them. Tumors shrank drastically, and 75% of treated mice survived the full 60-day study period. In contrast, control mice saw their tumors continue to grow, and all had died by the 20-day mark.
Intriguingly, Mito+ cells could multiply quickly and pass their extra mitochondria to the new cells. Other immune cells, such as lymphocytes and CAR-Ts, also showed improved cancer-killing abilities after receiving extra mitochondria.
"These supercharged T cells overcome one of the fundamental barriers of immunotherapy by penetrating the tumor and overcoming immune barren state in the tumor," said Shiladitya Sengupta, corresponding author of the study. "Mitochondria provide the fuel. It's like we're taking T cells to the fuel station and gassing them up. This transplanting of mitochondria is the dawn of organellar therapy – where an organelle is delivered to a cell to make it more effective."



