Breaking News
 Fearing US Reprisals, Mexico Halts Oil Shipment To Cuba
Fearing US Reprisals, Mexico Halts Oil Shipment To Cuba
 Iran Executes Suspected Israeli Spy In High-Stakes Act Of Defiance
Iran Executes Suspected Israeli Spy In High-Stakes Act Of Defiance
 TikTok Users Report Trouble Posting About Epstein, ICE, Days After Company Finalizes Sale...
TikTok Users Report Trouble Posting About Epstein, ICE, Days After Company Finalizes Sale...
 Chaos Is Spreading Like Cancer. What Happens Next?
Chaos Is Spreading Like Cancer. What Happens Next?
Top Tech News
 Researchers who discovered the master switch that prevents the human immune system...
Researchers who discovered the master switch that prevents the human immune system...
 The day of the tactical laser weapon arrives
The day of the tactical laser weapon arrives
 'ELITE': The Palantir App ICE Uses to Find Neighborhoods to Raid
'ELITE': The Palantir App ICE Uses to Find Neighborhoods to Raid
 Solar Just Took a Huge Leap Forward!- CallSun 215 Anti Shade Panel
Solar Just Took a Huge Leap Forward!- CallSun 215 Anti Shade Panel
 XAI Grok 4.20 and OpenAI GPT 5.2 Are Solving Significant Previously Unsolved Math Proofs
XAI Grok 4.20 and OpenAI GPT 5.2 Are Solving Significant Previously Unsolved Math Proofs
 Watch: World's fastest drone hits 408 mph to reclaim speed record
Watch: World's fastest drone hits 408 mph to reclaim speed record
 Ukrainian robot soldier holds off Russian forces by itself in six-week battle
Ukrainian robot soldier holds off Russian forces by itself in six-week battle
 NASA announces strongest evidence yet for ancient life on Mars
NASA announces strongest evidence yet for ancient life on Mars
 Caltech has successfully demonstrated wireless energy transfer...
Caltech has successfully demonstrated wireless energy transfer...
 The TZLA Plasma Files: The Secret Health Sovereignty Tech That Uncle Trump And The CIA Tried To Bury
The TZLA Plasma Files: The Secret Health Sovereignty Tech That Uncle Trump And The CIA Tried To Bury
The mitochondria are more than just the "powerhouse of the cell" – they initiate immune...
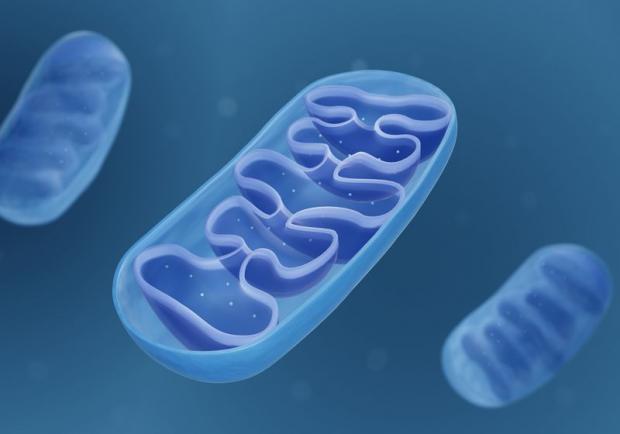
For decades, mitochondria have been relegated to the role of mere "powerhouses of the cell," churning out energy while the immune system's more glamorous players—white blood cells, antibodies, and cytokines—took center stage. But groundbreaking research is shattering this narrow view, revealing mitochondria as master regulators of immunity, orchestrating defenses against bacterial invaders with precision. Far from being passive energy factories, these tiny organelles act as cellular watchtowers, detecting microbial threats and triggering life-saving counterattacks. The implications are staggering: dysfunctional mitochondria may explain why autoimmune patients suffer recurrent infections, and boosting mitochondrial function could revolutionize infection treatment.
Key points:
Mitochondria act as metabolic sensors, detecting bacterial byproducts like lactate to initiate immune responses.
Neutrophils, the body's first responders, rely on mitochondrial signals to deploy sticky DNA traps (NETs) that ensnare and kill bacteria.
Dysfunctional mitochondria in lupus patients impair NET production, leaving them vulnerable to infections despite an overactive immune system.
The discovery opens doors for therapies that enhance mitochondrial sensing to fight infections or suppress harmful immune overreactions.
Nourishing the mitochondria with herbal medicines and phytonutrient-based therapies could empower patients struggling with compromised immune function.
The immune system's hidden command center
Neutrophils, the most abundant white blood cells, are the immune system's rapid-response team, rushing to infection sites to engulf and destroy pathogens. One of their deadliest weapons is the neutrophil extracellular trap (NET)—a spiderweb-like mesh of DNA and toxic proteins that traps bacteria like flies in amber. Until now, scientists believed NETs were triggered primarily by cellular damage. But new research reveals a far more sophisticated system: mitochondria act as metabolic spies, intercepting bacterial distress signals and ordering NET deployment.
The key to this communication? Lactate—a molecule long associated with muscle fatigue but now exposed as a bacterial SOS signal. Many pathogens, including Staphylococcus aureus, excrete lactate as they metabolize nutrients inside immune cells. When mitochondria detect this lactate, they sound the alarm, prompting neutrophils to eject NETs and expel the trapped microbes for other immune cells to finish off. Block this mitochondrial sensing, and bacteria slip through the defenses like thieves in the night.
When mitochondria fail: The autoimmune connection
This discovery sheds light on a cruel paradox: why patients with systemic lupus erythematosus (SLE)—a disease marked by hyperactive immunity—suffer relentless infections. The answer lies in their mitochondria. In lupus patients, these organelles grow deaf to bacterial lactate, failing to trigger NET production. The result? Pathogens replicate unchecked, while the immune system remains stuck in a self-destructive loop, attacking the body instead of invaders.